Babies First! and CaCoon services are crafted to be family-centered and flexible to meet the unique needs of the families and communities we serve. The Public Health Nurse (PHN) works in partnership with the client to co-create a plan of care to meet individual needs. The client’s plan of care is informed by the nursing process with the frequency of routine visits tailored to the client’s preferences, acuity and needs. The visiting schedule may also include a CHW if they provide case management according to the nursing plan of care. Regardless of the customized approach, all clients should receive:
- Initial Visit scheduled with the PHN
- Routine Visits scheduled with PHN, recommend a minimum of once a month (or every three months if a CHW is visiting monthly)
- Closing Visit scheduled with PHN
Model variation: CaCoon
The PHN may scale back contacts to as few as every three months if the family's situation or the child's condition has stabilized or requires only periodic monitoring.
Model variation: Community Health Worker (CHW)
A CHW can provide home visits in collaboration with a PHN by providing co-case management. A CHW may conduct client visits between nurse appointments to support the client based on the nursing care plan. This collaborative and flexible visitation model allows PHNs and CHWs to partner with families to determine the best visitation schedule. This ensures that the unique needs of each family are addressed, while aligning with the guidelines and standards set forth by both the Babies First! and CaCoon programs.
Initial Home Visit
For both Babies First! and CaCoon, the initial home visit should
be offered within one month of receiving the referral and should only be completed by a PHN. The nurse should plan for the initial visit to be up to two hours long.
In the instance where there is a waitlist and the initial home visit cannot be completed within one month of a client accepting a visit, the client should, at a minimum, be connected to OHP and a primary care provider. Referrals to other home visiting providers or community services is also recommended when possible.
The initial home visit is an opportunity to slowly get to know the family and should be client centered and client led. The PHN uses open ended questions and a soft touch to complete an initial needs assessment and create a nursing plan of care.
The items that a PHN must complete if the client/family accept services during the initial visit include:
- Program and services overview
- Agreement for services:
-
Informed consent for program and data collection
-
HIPAA, privacy, and communication agreements
- Any County/agency specific paperwork or policy
-
TCM Assessment/Plan, including establishing client
goals
HOPEful moments:
Every encounter is an opportunity to spotlight strengths within the family.
During the visit, celebrate moments of bonding and name PCEs you notice
Create a safe space by reminding families that sharing information is optional. Acknowledge they are not obligated to go into detail.
Close with positive and HOPEful messaging
Several assessments should be done within the first three visits to establish a relevant and applicable
nursing plan of care. These are listed in Activities Table 1 under the Frequency Recommendation of “Initial Visit".
Note:
Each client accepting services needs to complete an initial visit, including individual care plans and enrollment paperwork. Example: A PHN is enrolling a parent and baby at an initial home visit. The nurse will provide one program and service overview but will need the parent to sign two sets of program consents, one for themselves, and one for the baby.
Minor Consent
Youth aged 15 years and older must consent to receive services. In Oregon, the legal age for giving consent to care is 15. There are no specific laws for CYSHCN nor for youth with physical or intellectual disabilities. This means that you would follow consent processes just as you would for any other youth. Youth enrolled in a program prior to their 15th birthday should sign consents by their 15th birthday to continue receiving services.
Though Oregon law does not give minors a "right" to confidentiality nor parents a "right" to disclosure,
it is recommended that youth 15 and older sign a release of information form permitting parents to discuss their youth's health needs with home visiting staff. More information regarding minor consent and confidentiality from the Oregon Health Authority can be found
here. Frequently asked questions on working with clients in DHS custody can be found
here.
CaCoon and Babies First! staff can encourage families to start a conversation with their youth regarding HIPAA laws and confidentiality. They can explore who will provide decision-making support if the youth needs or desires it. CaCoon staff can support the family in understanding the youth's ability to understand and provide informed consent. Evaluation of the youth's capacity to consent is an essential step in promoting their autonomy and involvement in their healthcare decision-making process. It is crucial to educate and support youth before signing consent and release of information documents so that they understand what consent and confidentiality mean. This practice aligns with
Supported Decision Making practices and promotes informed healthcare decision-making for transition-aged youth.
Routine Visit Schedule
The PHN and client/family decide the frequency of routine visits when they create the plan of care together. The routine visit schedule is centered on the client's preference but should also consider the PHN acuity assessment, nursing diagnoses, client needs, and best practice recommendations based on population. It is likely that frequency of visits will fluctuate during the client's enrollment and as the client begins to utilize needed services or develops additional needs.
In general, it is recommended that
all clients/families be offered monthly visits. Evidence shows that frequency of visits has a positive effect on child development (11). Other evidenced based models have
shown measurable outcomes using frameworks of frequent visiting.
Client factors that affect visit frequency include, but are not limited to family preference, client's medical home status, whether community support is established, and if the client will have an anticipated increase or decrease in needs based on family or client age/stage.
Best practice guidelines based on the client population also affects visit frequency. For instance, it is best practice to provide a home visit for a newborn baby within 2 weeks of birth; therefore, it would not be appropriate to visit this client every 2 months. On the other hand, a 2-to-3-month schedule may be appropriate with a CaCoon client who has established support from Early Intervention (EI) with an Individualized Family Service Plan (IFSP). For more on population-specific frequency, please review the applicable activity table, links to clinical guidelines, and review the THEO collection schedule.
Assessment and THEO Data Collection Schedule
While the frequency of visits should be customized to align with the specific needs of each family, it's important to note that
best practice guides timeliness of activities like
developmental assessments, client screenings and education. The state data collection schedule is meant to align with typically expected case management activities based on the client's age or developmental stage.
Every visit should be documented in THEO using the Every Visit Survey. The THEO data collection schedule below identifies additional data that should be entered. This data collection schedule should be considered when determining the timing of visits and completion of other data collection surveys.
THEO Data Schedule
Prenatal: 32-40 weeks
Postpartum: 1-8 weeks, 6 months, and 1 year
Infant and Young Child: Birth-2 months, 6, 8, 12, 18, 24, 30, 36, 42, 48, and 54 months
Child and Youth: Every 6 months
Parent/Caregiver: Every 6 months
Model variation: CHW
Either a CHW or a PHN may complete the data collection surveys; however, if a CHW has not been competency validated and assigned to conduct specific assessments (e.g., ASQ), they will not be able to complete the full Periodic Assessments (such as the Infant and Child Survey or Child/Youth Survey). In instances where these comprehensive surveys are due, we strongly recommend that the visit be scheduled with a PHN to ensure complete an accurate data collection.
Closing Visits
When a family is prepared to transition out of the program, a final visit should be conducted by the PHN. Ideally, subsequent needs and referrals for transition out of the program would be addressed at previous visits and the last visit is a home visit used to celebrate or “graduate" out of the program. Give thought to other programs and community resources that can serve as supports for the client and family after they are ready to leave the program. Making those connections before discharge can smooth the transition and minimize risk of interrupting their momentum. This is sometimes called a “warm hand-off."
Outlined below are considerations to help home visitors in determining how ready a family is for closure. This is not meant to be a checklist and families don't need to meet all criteria.
Perinatal people enrolled during pregnancy
Consider graduation from the Babies First! Program if:
- A post-partum check-up has been completed
- A Reproductive Health Plan is in place
- There are no concerns about mental health, or mental health services are in place.
- There are no concerns about substance use, or support/treatment services are in place.
- A support system has been identified.
- Breastfeeding is going well, or other feeding plan is in place.
- A primary care provider/medical home has been established.
- A TCM Assessment shows that the client does not need services or declines assistance accessing and/or utilizing needed services.
Infants and children
Consider discharge from the Babies First! Program if:
- A primary care provider/medical home has been established.
- A support system has been identified.
- No concerns about growth and development.
- No concerns about child safety.
- No concerns about parent child interaction.
- A primary care provider/medical home has been established.
- A TCM Assessment (See Chapter 4) shows that the client does not need services or declines assistance accessing and/or utilizing needed services.
When continuing to maintain a client on the Babies First! Program beyond two years, seek the advice of your supervisor. Discuss transition plans with the family and review clear goals and timelines.
At times, closure of a case happens abruptly; for instance, if a family moves or does not make contact again (lost to follow up). There are many scenarios that make it difficult to “celebrate" the case closure or where a visit in the home is not possible. In these cases, it is still important to make a good faith effort to have a final visit (e.g., via telephone) with clients to address any unmet needs and, if possible, refer for alternative support. If a final visit is not possible,
case closure must be documented in the client's medical chart and a Discharge Letter sent to the client. It is recommended to
discharge clients who have not been visited in three months (unless visits every 3-6 months is in the care plan). If clients are willing to re-engage later, they may be re-enrolled in the program.
If a final visit is possible, below are some topic ideas for a strength-based closure visit:
Note: Example
“One goal was to make it to your postpartum appointment, and you did it! That is no small feat while recovering! I commend you for taking care of yourself in that way."
Note: Example next steps
“So, this is our last visit, can you tell me how you're feeling about this next stage? And let's review who you'll reach out to after today." Followed by, “So let me recap your plan. [Child] is enrolled in Head Start and you have great support from them and your pediatrician. Moving forward, if you have healthcare related questions, your plan is to contact your PCP or send a message through MyChart. And for other community support, your Family Support Specialist can help you at Head Start. Is that correct?" followed by “At any point if you find yourself needing more support for some reason, please contact us and we can explore if opening your case again would be helpful. Do you still have my contact information?"
Have you explored long term planning with the caregiver/adult client about professional development and self-sufficiency?
- “Do you picture yourself back in the workforce at some point? If so, do you have an interest we could explore?"
- Have you considered work training/support or going back to school? You qualify for benefits being a parent. Do you know about Financial Aid?
- Have you thought about establishing Credit or exploring debt relief?
- Does the parent qualify or possibly qualify for DD services or TANF even if they are not accessing?
Do they anticipate, and are they planning for, the child's next development phase or life transition?
- Transfer to kindergarten or schools (ex: IFSP to IEP)
- Are they able to complete an ASQ and ASQ-SE independently and advocate for needed services?
- Can they verbalize the safety issues with the next age/stages?
- Example: learning to crawl/walk and needing to babyproof
- Transitioning to solids and learning about choking hazards and family style eating
- Preparing for the transition to preschool or kindergarten
- Do they have family rules and routines established?
- Have you explored discipline techniques and what to do when there is conflict?
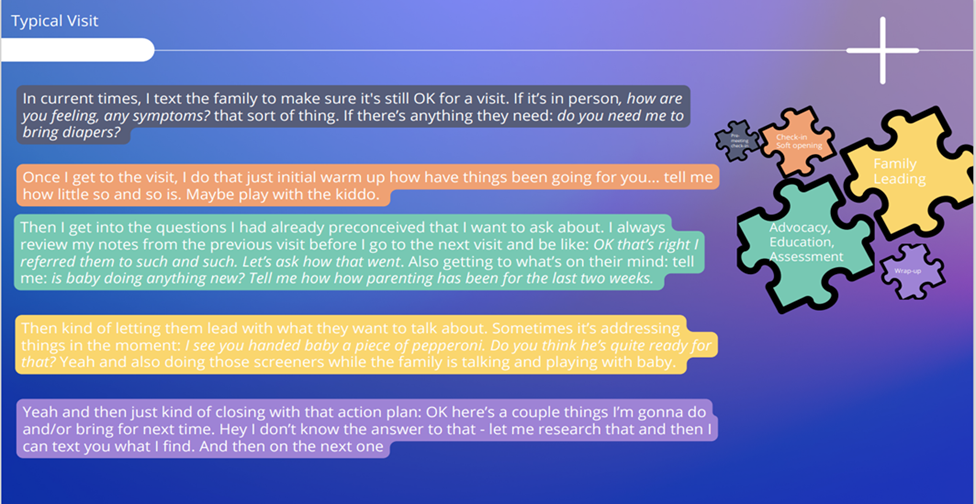
Routine Visit Structure
The Babies First! and CaCoon programs are crafted to be family centered programs with visit structure consisting of activities and topics informed by evidenced-based best practice and client interests. The
2023 Babies First! Program Evaluation highlights that while program implementation can look very different across Oregon's counties (staffing, population reach, etc.)
there is a fundamental structure of a visit that consists of 5 main pieces.
Best Practice: Meeting Structure
Pre-meeting check-in
Check-in soft opening
Assessment, Education and Advocacy (also known as Care Coordination and Case Management)
Family Leading
Wrap-up
These 5 pieces can be thought of as puzzle pieces that are changing in size at each visit. Using the pieces does not have an order (non-linear), and all the pieces may not be used together at every visit. These pieces are consistently implemented with family empowerment at the core.

Using the 5 pieces of a home visit: in the words of a Babes First! Nurse Home Visitor
Pre-Meeting Check-in
- Appointment reminder
- Home Visitor preparation:
- Chart review
- Gathering anticipated materials –educational handouts, referral forms, HV supplies
- Client screen for symptoms of illness (e.g., cough or sore throat), as indicated by local and state policy for infection control.
Nurse bags should contain stethoscope, BP cuff, thermometer, eye pen light, basic first aid kit (such as available from a grocery store), weight machine, and length measure. Optionally, it may have cleanable toys.
Check-in Soft Opening
Entering a neighborhood and household is always a time to do a quick and friendly safety check. Usually, this starts by introducing yourself and asking permission to enter or proceed with visit (even if it's implied, and even if you have been there multiple times). When entering a household, it's always a good idea to greet everyone present. This helps you know who else is in the house, promote community engagement, and can
support the client with transitioning into the visit safely.
Set the stage
- Offer non-choking toys, or for older children, coloring or puzzle
- If a TV is on, ask permission to turn it off. Consider using this opportunity to engage in teachable moments, parallel play with the child, and promoting parent/child interaction and bonding.
- Ask permission and then set out prompts for the activity on the visit schedule, like a baby scale, blood pressure cuff, or educational material you are planning to share. This acts as a visual to identify the next task that is coming during the visit.
- Use the
FAN approach
- Start with routine opening questions that center the client
- Check in about “in the moment" needs.
Case Management/ Care Coordination
After a soft check-in, home visitors may use a variety of technique to keep the visit client centered and conversational in format. This collaborative process of using the nursing process for assessments, planning and interventions is also known as case management, and often used interchangeably with the term care coordination.
Care coordination involves deliberately organizing patient care activities and sharing information among all the participants concerned with a patient's care to achieve safer and more effective care (Agency for Healthcare Research and Quality). Care coordination is identified by the Institute of Medicine as a key strategy that has the potential to improve the effectiveness, safety, and efficiency of the American health care system. Well-designed, targeted care coordination that is delivered to the right people can improve outcomes for everyone: patients, providers, and payers. The Babies First! and CaCoon programs have utilized an approach that incorporates evidence informed Nurse home visiting activities with Targeted Case Management.
“Home visiting activities" is a family centered way we can define some of the nurse case management interventions. These activities can be filtered into three broad buckets:
- Assessments
- Education, and
- Advocacy
Key Activities

Assessment, Education, Advocacy: These three broad terms are often used to refer to other PHN interventions listed in
Figure 1. For more details about specific nursing interventions and evidence that guides these activities, please review
Public Health Interventions: Applications for Public Health Nursing Practice.
Assessment
Every enrolled client needs an
initial nursing assessment and plan completed and documented. It is important to note that some assessments, like breastfeeding or environmental exposure, may overlap for your clients. In these cases, an overarching assessment is appropriate, but individual client assessment should also be documented.
HOPE informed:
Prepare the family for any assessments by explaining the kinds of questions you will be asking and why.
Screenings and assessments often highlight "problems" and the need for "intervention". Consider using strength-based language instead.
Always remind clients that screenings and assessments are optional. Embed time for questions.
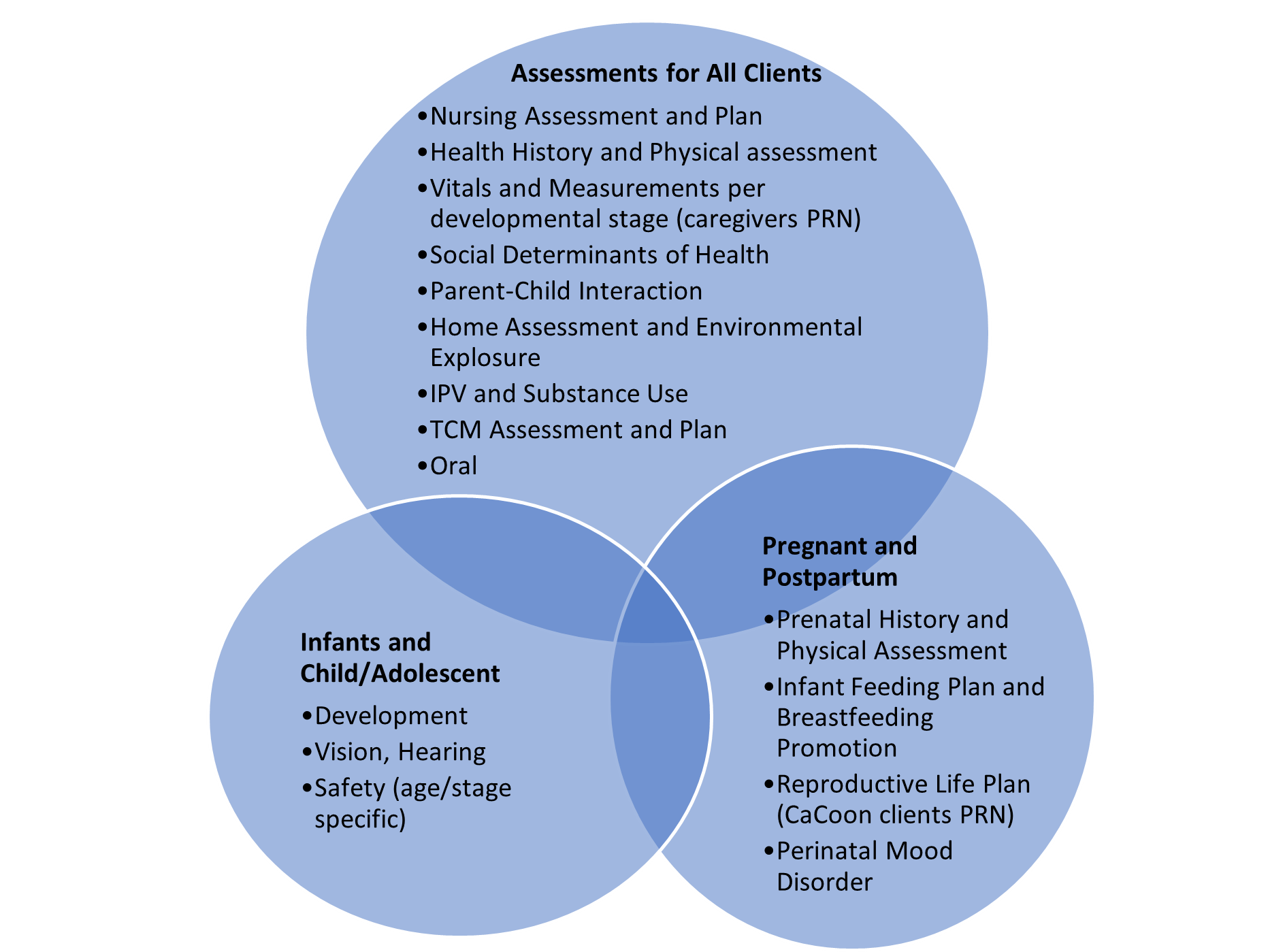
Figure 4 below shows major assessment topics by population groups. Likewise, the
Activities Section Table 1 (further below on this page) includes a detailed chart of assessment by population and frequency. Assessments should be done in a HOPE-informed way.
Figure 4: Major assessment topics by population group
Model Variation: CHW
All CHWs partner with the nurses and clients to provide education and navigation support with resources and referrals. If trained, competency validated, and assigned tasks by the Nurse Case Manager, the CHW may also complete tasks such as taking blood pressures or weights. The nurse must maintain knowledge of client progress by reviewing the CHW notes after every visit.
Education
According to Oxford dictionary,
education is defined as “an enlightening experience." For the purposes of home visiting, client education occurs during “educational moments" when the client is engaged and participating with the home visitor in learning.
The Public Health Nursing Wheel defines some of these moments more specifically as: Counseling, Health Teaching, and Consultation. For instance, Counseling is defined as “establishing an interpersonal relationship at an emotional level, with the goal of increased or enhanced capacity for self-care and coping" and “explores the emotional response to integrating new health information into life's circumstances" (pg. 142).
Recommended topics to address by population (e.g., pregnancy, post-partum, childhood) are covered in
Activities Section Table 1 (scroll down to view table).
Advocacy
Advocacy is defined by
Public Health Interventions: Applications for Public Health Nursing Practice manual as the act of promoting and protecting the health of individual and communities by collaborating with relevant stakeholders, facilitating access to health and social services, and actively engaging key decision-makers to support and enact policies to improve community health outcomes. Possible advocacy roles are:
-
Accompanying: Speaking with people
-
Representative: Speaking for people
-
Empowering: Enabling people to speak for themselves
-
Mediating: Facilitating communication between people
-
Modeling: Demonstrating practice to people and policymakers
-
Negotiating: Bargaining with those in power
-
Networking: Building coalitions with other individuals or organizations
This definition of advocacy embodies the foundation from where a Nurse provides care coordination and case management through home visiting. Advocacy is used as a Nursing intervention after partnering with the client to assess needs to determine next steps.
Major components of care coordination involve ensuring that families are aware of services and how to access them. The care coordinator should be familiar with a wide range of community resources, including (but not limited to):
- Primary, secondary and tertiary health care (including mental health and behavioral health services)
- Speech, language, vision and hearing resources; early intervention programs
- Respite care and childcare services
- Financial assistance programs
- Parent groups
- Advocacy groups
- Transportation services
- Local, state and federal offices
HOPEful Moment: Referrals
Celebrate what the family is already doing for PCEs in the area you are referring for.
E.g., Early Intervention referral for ASQ follow up for communication.
Highlight what the family is currently doing to support communication development.
“I see you have children's books available, and it sounds like you are reading with (child) every day. This is fantastic for development! And when (child) is listening to you read or sing, they are learning 'receptive language'. These are all important piece you are already doing! This referral may simply help give us ideas about more support and helpful tips."
Referring families to services involves much more than just giving families a brochure or number to call or a form to fill out. They may need information, support and/or follow up to navigate services and comfortably make decisions about care. In addition, the nurse or CHW need to be certain that the agency to which the family is being referred is the right one to meet the need (are they accepting clients? Are they trauma informed?). More harm than good will be done by referring already stressed families to an agency whose services do not or will not match the need. Provide follow up for families to ensure they are not experiencing barriers in receiving services to which they have been referred.
An identification of new barriers usually indicates a need for additional assessment, documentation, and possible change or shift in goals.
Best Practice: Trauma Informed Care
More harm than good will be done by referring already stressed families to an agency whose services do not or will not match the need.
The nurse or CHW need to be certain that the agency to which the family is being referred is the right one to meet the need (are they accepting clients? Are they trauma informed?)
Family Leading
Family leading is at the heart client centered case management for our home visiting programs. This trauma informed approach explores and appreciates the client and family perspective of health and needs. This approach also demands that the home visiting staff and program agency have a practice in exploring and supporting cultural humility and addressing implicit and explicit bias.
Ways home visitors can support clients/families:
Wrap Up
The end of each home visit should include a
summary of home visiting activities, what the client has or wants to accomplish, what both the client and home visitor have agreed to do, and the planned topics for the next visit. This is also a good time to schedule or confirm the next visit time and plan for follow up from the nurse and/or CHW. Encouraging the client to provide teach back and reviewing emergency plans between visits is also recommend.
Wrap Up Documentation Example:
Client will reach out to Nurse or CHW with any questions or concerns about plan but will contact doctor, 911, or go to emergency room for any urgent health matter. Client verbalizes understanding and agreeable to plan with next visit scheduled for 4 weeks (put exact date)
Activity Tables by Population
HOPEful moment:
Prepare your client for screenings by providing information beforehand:
Explain the screener and the kinds of questions you will be asking.
Explain why you are conducting the screening.
Remind family that this is optional.
Schedule for a time in the future when parent can feel prepared to discuss.
The major population groups are:
- Prenatal
- Postpartum (up to one year post birth)
- Newborn (under 1)
- Young Child (1-5 years of age)
- Child/Youth (5-21 years of age)
- Caregiver
- Community
Table 1. Activities Table
Table 1 includes a detailed chart of required assessment by population and frequency.
Please refer to the Nurse Home Visiting Clinical Guidelines for guidance on specific assessments.
Use the Search bar to limit table, such as for specific populations or topics. Click on + for helpful links for each topic.
Additional Health Education Topics and Resources
HOPEful moment:
When you screen:
Briefly review power of the brain to change.
Review science of Positive Childhood Experiences and the power to offset health outcomes.
Create a safe space to share, acknowledging that parent should not feel obligated to go into detail.
Conduct screener or assessment.
HOPEful moment:
After you screen:
Review PCEs that you have witnessed in the family.
Celebrate with the parent the work they are already doing to create resilience and health for their children.
Ask parent if they are interested in brainstorming more ways to create PCEs for children.
Close with positive, HOPEful messaging.
Working with Interpreters
Interpretation services must be provided to all clients with limited English proficiency. All people acting as interpreters must be certified by the Oregon Health Authority, per House Bill 2359. See this
website for more details. A CHW may act as an interpreter at a visit if they are certified and competency validated to do so. Use best practices for working with interpreters: detailed information on best practices can be found at the
Center for Excellence of for Immigrant Child Health and Well Being,
9 Best Practices for Using an Interpreter for ASQ, and
Association of American Medical Colleges Guidelines for Use of Medical Interpreter Services.
Return to top
Considerations for CaCoon or clients with disabilities and/or special health care needs
Please Note: While the CaCoon program is specifically designed to support children and youth with special healthcare needs (CYSHCN) in Oregon, Babies First! may also serve clients (parents or children), who have disabilities or special healthcare needs. Therefore, the guidelines and considerations outlined in this section are equally applicable to families and Home Visitors involved in both CaCoon and Babies First! Programs.
This section focuses on some of the unique considerations required for providing high-quality, evidence-based care to this population. The guidance provided aligns with the
National Care Coordination Standards for CYSHCN. The National Care Coordination Standards for Children and Youth with Special Health Care Needs (CYSHCN) serve as a critical framework for guiding high-quality care delivery to this vulnerable population. Published in 2020 by the National Academy of State Health Policy, these standards are designed to ensure that care coordination for CYSHCN is consistent, evidence-based, and holistic. They are anchored in foundational principles that emphasize health equity, family involvement, cultural competence, and the use of evidence-based practices. These standards are of paramount importance because they offer a unified approach for healthcare professionals, enabling effective collaboration across various sectors including medical, educational, behavioral, and social services.
There are 6 Domains:
Screening, Identification, and Assessment
This domain focuses on the early and accurate identification of special health care needs through various screening methods and assessments. It sets the foundation for all subsequent care.
Shared Plan of Care
This domain emphasizes the development of a comprehensive, family-centered care plan that is shared among all stakeholders, including healthcare providers, educators, and family members. The plan outlines the objectives, roles, and responsibilities for each party involved.
Team-Based Communication
This area stresses the importance of effective and open communication among all team members involved in a child's care. It ensures that everyone is on the same page and collaboratively working towards the child's well-being.
Child and Family Empowerment and Skills Development
This domain aims to actively involve families in the care process and empower them with the necessary skills and knowledge to manage their child's condition effectively.
Care Coordination Workforce
This domain deals with the training, skill set, and continuous development of the healthcare workforce involved in coordinating care for CYSHCN. It underscores the need for professionals to be well-versed in best practices and emerging trends.
Care Transitions
This last domain addresses the challenges and strategies involved when CYSHCN move from one care setting to another, such as from pediatric to adult healthcare, or from school to the workplace. It highlights the importance of a smooth and well-prepared transition to avoid gaps in care and maintain optimal health outcomes.
Understanding these domains enables home visitors to provide more comprehensive, effective, and coordinated care for CYSHCN and their families. You can read more in depth about these Standards
here.
Core Knowledge
Home Visitors need not be experts in every disability or chronic condition, but they should be knowledgeable about commonly occurring ones, understanding their potential impacts on child and family development. Home Visitors should know how to connect families with the appropriate specialists and resources.
Understanding the “diagnostic odyssey"
The journey to diagnose a child's disability or special health care needs varies greatly among families, both in how it begins and how it unfolds. For some, the process starts as early as during pregnancy, while for others, it might occur later in life due to an injury or noticeable developmental delays. This period of seeking answers is often termed the "diagnostic odyssey," a phase that can be emotionally taxing and prolonged, sometimes stretching over weeks, months, or even years. In some instances, families never arrive at a definitive diagnosis. The path of this diagnostic journey is highly individualized; some families may opt not to pursue a diagnosis at all, or to delay the quest for answers until their child is older. Home visitors can play a crucial role in supporting families during the "diagnostic odyssey." With their unique vantage point into the family's day-to-day life, home visitors can offer emotional support, share observations, and provide valuable resources or referrals to specialized services. They can also help families navigate the complex healthcare system by assisting with paperwork, offering guidance on questions to ask healthcare providers, or even attending medical appointments to serve as an advocate for the family. By providing a consistent presence and a knowledgeable perspective, home visitors can help alleviate some of the stress and uncertainty that families experience during this challenging time. Moreover, they can empower families with the tools and information they need to make informed decisions, whether that means pursuing further diagnostic tests or considering alternative support services.
Importance of a “Medical Home"
The concept of a Medical Home, particularly a Patient-Centered Primary Care Home (PCPCH), is of immense significance for people with disabilities and special healthcare needs. Given the higher frequency of appointments, medications, and treatments required by CYSHCN, a strong, collaborative relationship with a primary care provider is essential for coordinating and managing care effectively. The elements of a PCPCH, such as accessibility, accountability, comprehensiveness, continuity, and coordination, serve to streamline this process and ensure that families receive the holistic care they deserve.

Home visitors can act as crucial facilitators in helping families access and maintain a Medical Home. Because of inequities, economics, and other social determinants of health, not all families will have access to a permanent primary care provider. Home visitors can help identify and bridge this gap for families by participating in conversations about community needs, advocating for more support, discussing obstacles with local health care administrators, and helping reduce barriers to care. To learn more about PCPCH click
here.
Importance of Cross-Systems Care Coordination
Cross-systems care coordination is essential for children and youth with special healthcare needs (CYSHCN) because their care often involves multiple sectors, such as healthcare, education, social services, and behavioral health. Effective coordination among these diverse systems is crucial for holistic care and optimal health outcomes. It helps to prevent the fragmentation or duplication of services, eases the family's burden of navigating complex care networks, and ultimately promotes a more efficient and impactful approach to care. Home visitors play a pivotal role in this coordination. They act as a liaison between the family and various service providers, helping to bridge gaps in communication and understanding. With their unique vantage point—being familiar with both the family's needs and the offerings of different systems—home visitors can identify potential resources, make referrals, and assist in developing a comprehensive, shared care plan. Through regular home visits, they can also monitor how well services are being coordinated and where adjustments may be needed, ensuring that the child's care remains cohesive across all involved systems.
A child's care team may be diverse, including doctors, therapists, public health nurses, home visitors, case managers, school staff, social workers, interpreters, and others. Given the diversity and potential complexity, effective cross-systems care coordination becomes paramount. You can help families create and manage a
care map, which can serve as a visual guide to keep track of all providers involved in their child's care.
Leveling Up with Shared Care Planning
Shared care plans are pivotal in establishing a structured, yet flexible roadmap for families and professionals who are collectively working to meet the healthcare needs of a child. Unlike other types of care plans, shared care plans are collaborative documents that spell out families' goals and articulate how these objectives will be reached. These comprehensive documents often include key components such as the child's brief medical history, strengths and assets, current and past interventions or treatments, recommendations, preferences, and most importantly, a well-defined plan of action specifying roles, responsibilities, and timelines.
In instances where children may have multiple care plans from different organizations, it's crucial to cross-reference these documents to ensure consistency and avoid duplication of efforts or contradictory recommendations. As a home visitor, you can facilitate this process by asking families for copies of all existing care plans. You have a unique opportunity to identify overlaps and gaps, and to liaise with other service providers to harmonize the various plans. Such coordination ensures a more cohesive, effective approach to care, eliminating redundancies and aligning efforts toward common objectives. If you notice the potential for such alignment, it's important to communicate this opportunity to your supervisors for further action.
Shared care planning, therefore, is not just a document; it is a dynamic process that fosters communication, collaboration, and shared responsibility among all stakeholders. It empowers families and streamlines the care journey, making it a vital tool in the management of children with special healthcare needs. For more information on shared care planning click
here.
Transition Support
Transition support is an essential component of care coordination for CYSHCN. Transition here refers to the crucial shift from pediatric, family-centered healthcare to adult, patient-centered healthcare. This transition process usually kicks off around the age of 14 and can extend through ages 18, 21, or even older. It involves not just changing healthcare providers—from a pediatrician to an adult-focused provider like a family practitioner—but also equipping the young adult with the skills needed to independently manage their healthcare.
Contrary to popular belief, young adults with disabilities don't indefinitely continue to see their pediatricians. Even if they are unable to manage their own care, there will be a point when transitioning to an adult healthcare provider becomes necessary. This process requires thoughtful planning and effort, which is where home visitors play an invaluable role.
Home visitors can start by helping families understand their current pediatric clinic's transition policies.
Around the age of 14, families should be encouraged to inquire about the anticipated age for transition and the preparations required. Home visitors can also utilize tools like the transition checklists developed by
Got Transition, a part of The National Alliance to Advance Adolescent Health. These checklists can be reviewed periodically to monitor progress and can serve as discussion aids during medical visits.
The
Oregon Family-to-Family Health Information Center also provides many resources
for families and professionals navigating the health care transition process.
Transition support is more than a mere administrative change; it's a complex process that demands emotional, cognitive, and logistical preparation. Your role as a home visitor can facilitate this process, ensuring a smoother, more prepared transition that sets the stage for young adults to take ownership of their health in a new healthcare setting.
Additional Training for working with clients with disabilities and/or special healthcare needs
OCCYSHN developed a self-paced, online course for Community Health Workers, to train them on addressing the particular needs of CYSHCN and their families.
Supporting Families: Navigating Care and Services for Children with Special Health Needs teaches the fundamentals of partnering with Oregon families to get what they need for their children's health and development. While the course is part of a larger Community Health Worker program, it is also available as a stand-alone training. While OCCYSHN initially designed it for CHWs, the content is relevant to a variety of professionals who work with CYSHCN, including pediatric care coordinators, home visitors, family navigators, and case managers. If you haven't already taken the course, we highly recommend doing so to enhance your skills and understanding in this critical area. Home visitors interested in taking the course can contact OCCYSHN at
occyshn@ohsu.edu to request access at no cost.
Return to topPlease let us know if you have suggestions, any links are broken, or if any information is outdated.
Babies First! and CaCoon Manual Feedback Form