1. Logic Model
Babies First! Logic Model
CaCoon Logic Model
**In development**
2. Program Objectives
Babies First!:
The Babies First! program is a relationship and strength-based public health nurse home visiting program that partners with families to improve pregnancy, family and child health outcomes, and to connect to quality health care and the community supports they deserve.
CaCoon:
See the
CaCoon Program Standards
CaCoon is a relationship and strength-based public health nurse home visiting program that partners with families with children and youth with disabilities or special health care needs by supporting them to access and coordinate quality health care and the community supports they deserve.
Return to Top
3. Eligibility Criteria
Babies First!:
The Babies First! Program provides services to perinatal people, infants and children through four years of age, and parent or primary caregivers (also known as caregiver relatives but referred to as “caregivers" in this manual) of eligible children.
Local programs are encouraged to assess the needs in their community, as well as their program capacity, and target a specific population within the eligibility lists. Please inform a MCH Nurse Consultant of these plans.
CaCoon Criteria:
The Maternal and Child Health Bureau (MCHB) defines children and youth with special health care needs (CYSHCN) as “children who have or are at increased risk for chronic physical, developmental, behavioral, or emotional conditions. They also require health and related services of a type or amount beyond that required by children generally."
According to the MCHB
National Survey of Children's Health (NSCH), in our country:
- About 14 million children under 18 years old (19%) have a special healthcare need.
- 25% of homes had one or more children with a special healthcare need.
- CYSHCN are more likely to live in poverty, be non-Hispanic Black, and have public insurance than non-CYSHCN.
CaCoon program services are available to:
- Any child, birth through 20 years of age (up to their 21st birthday), who fits the above definition and has a diagnosis detailed in Targeted Case Management (TCM)
OAR 410-138-0040 “Diagnosis" column of
Table 2.
- A parent (primary caregiver) of an enrolled child or youth may also be enrolled in the CaCoon program (See 410-138-0020).
- Children and their families are seen without regard to economic status.
Local programs are encouraged to assess the needs in their community, as well as their program capacity, and target a specific population within the eligibility lists.
4. Roles
Administrator:
The public health administrator or program manager should
- Provide adequate resources to nurse supervisors to maintain minimum program standards (e.g., reflective supervision, case conferencing, team meetings, outreach/referral building).
- Know about funding sources used in the public health system to provide public health nursing services (e.g., Targeted Case Management, Administrative and Public Health Medicaid Match, modernization funds, Coordinate Care Organization funds).
- Advocate for provision of home visiting services in the community. Examples:
- Support the development of a community advisory board that addresses home visiting systems issues.
- Attend home visiting network/coordinating meetings.
- Support centralized referral networking.
Supervisor:
The Babies First! and CaCoon Supervisor has many duties. They may keep a small (1-2 family) caseload per 1 FTE dedicated to Supervision, as needed. The supervisor's main duties include:
- Provide clinical oversight and support of home visitors through case conferencing, chart reviews and joint visits:
- two hours of case conferencing per month (see Program Administration section below)
- four charts reviewed per home visitor per year (per privacy officer, peer chart review is acceptable for the purposes of quality assurance), and
- one observed home visit per home visitor per year
- Provide reflective supervision (RS) to each home visitor two hours per month per home visitor, one hour of which may be from group reflective supervision or peer reflective supervision.
- Lead at least monthly team meetings: ensure home visit staff are up to date on clinical and program guidelines, nursing, CHW and home visiting best practices.
- Maintain county-specific guidelines and protocols.
- Establish and support orientation of new staff, including understanding and support in work between CHW and PHNs, as applicable.
- Ensure professional development opportunities of team.
- Participate in RS training/professional development.
- Develop, maintain, update nursing documentation processes.
- Stay up to date on all program guidelines and ensure they are incorporated into nursing (and CHW practice as applicable).
- Outreach and referral development
- maintain positive relationships with home visiting and community system partners.
- visit referral partners at least every three months to present to partners.
- develop/ distribute marketing materials.
- participate in community partner meetings
- participate in community events (e.g., tabling at local fair)
- Review data and reports to support program continuous quality improvement and quality assurance.
- Meet monthly with designated State Nurse Consultant. These monthly phone calls will include updates, information sharing, and program support from the MCH Nurse Consultant*.
*For Supervisors working in both the Nurse-Family Partnership and Babies First! or CaCoon home visiting programs, contact a MCH Nurse Consultant for discussion of requirement.
Nurse:
The minimum required staffing for an implementing agency is at least a total FTE of 0.5 PHN. BSN prepared nurses are preferred but not required. If a local program is unable to meet the minimum staffing or caseload requirement, contact a Nurse Consultant for discussion.
Nurse home visitor job duties do not just include home visits: PHNs must prepare for visits, work on case management activities in between visits, document visits, commit to continuing education, attend community meetings, and participate in reflective supervision, case conferences and team meetings.
Community Health Worker:
A CHW is a frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community served. The Babies First! and CaCoon Programs may include CHW staff whose role is to provide health education and case management services to meet the client goals according to the plan developed by the PHN. CHW productivity standards are the same as the PHN.
See Appendix D for guidelines on how CHWs and PHN work together, including the role of CHWs for interpretation services.
Support/Clerical Staff:
Support or clerical staff may work with PHN and CHW on a variety of program administrative tasks.
These include, but are not limited to:
- Scheduling client appointments
- Data entry (e.g., THEO data collection forms)
- Printing/packaging client materials
- Printing/packaging assessment and data collection materials for home visitors
- Review and follow up on required surveys
It is highly encouraged that implementing agencies allocate at least 0.2 support staff FTE per HV FTE for home visiting programs.
Return to Top
5. Program Administration
Meetings
Case Conferencing:
Home visitors are asked to share a specific client situation that they would like to reflect upon. The team supports the home visitor in reflecting on what went well and what can be learned and applied in the future. The Gibbs Reflective Cycle is used to facilitate the conversation.
Best Practice: The Gibbs' reflective cycle is a process involving six steps:
Description - What happened?
Feelings - What did you think and feel about it?
Evaluation - What were the positives and negatives? How did you strengthen each HOPE domain?
Analysis - What sense can you make of it?
Conclusion - What else could you have done?
Action Plan - What will you do next time? It is a 'cycle' because the action you take in the final stage will feed back into the first stage, beginning the process again.
Reflective Supervision:
Each home visitor is required to receive two hours of reflective supervision per month (regardless of FTE).
See
Chapter 3 for details on reflective supervision.
See Appendix E for supporting material for reflective supervision sessions.
Team Meetings:
All Babies First! and CaCoon Programs are required to have monthly team meetings at a minimum (Triennial Review Tool item). Team meetings topics may cover administrative items, outreach/referral, nursing practice, professional development, manual/clinical guideline review, etc. Two hours per month of team meetings may be devoted to case conferencing, or case conferencing may be scheduled separately.
Return to Top
6. Documentation
Also see,
Documentation Checklist in Appendix G.
Medical Record
Medical records must have the following documentation completed within two business days of a visit: Nursing Plan of Care or CHW visit documentation, as applicable.
The nursing plan of care must include the following information:
- Subjective data
- Objective data (specific data that must be included at a minimum is delineated in the Triennial Review Records Review Tool)
- Assessments (see Chapter 6 and the Triennial Review Records Review Tool)
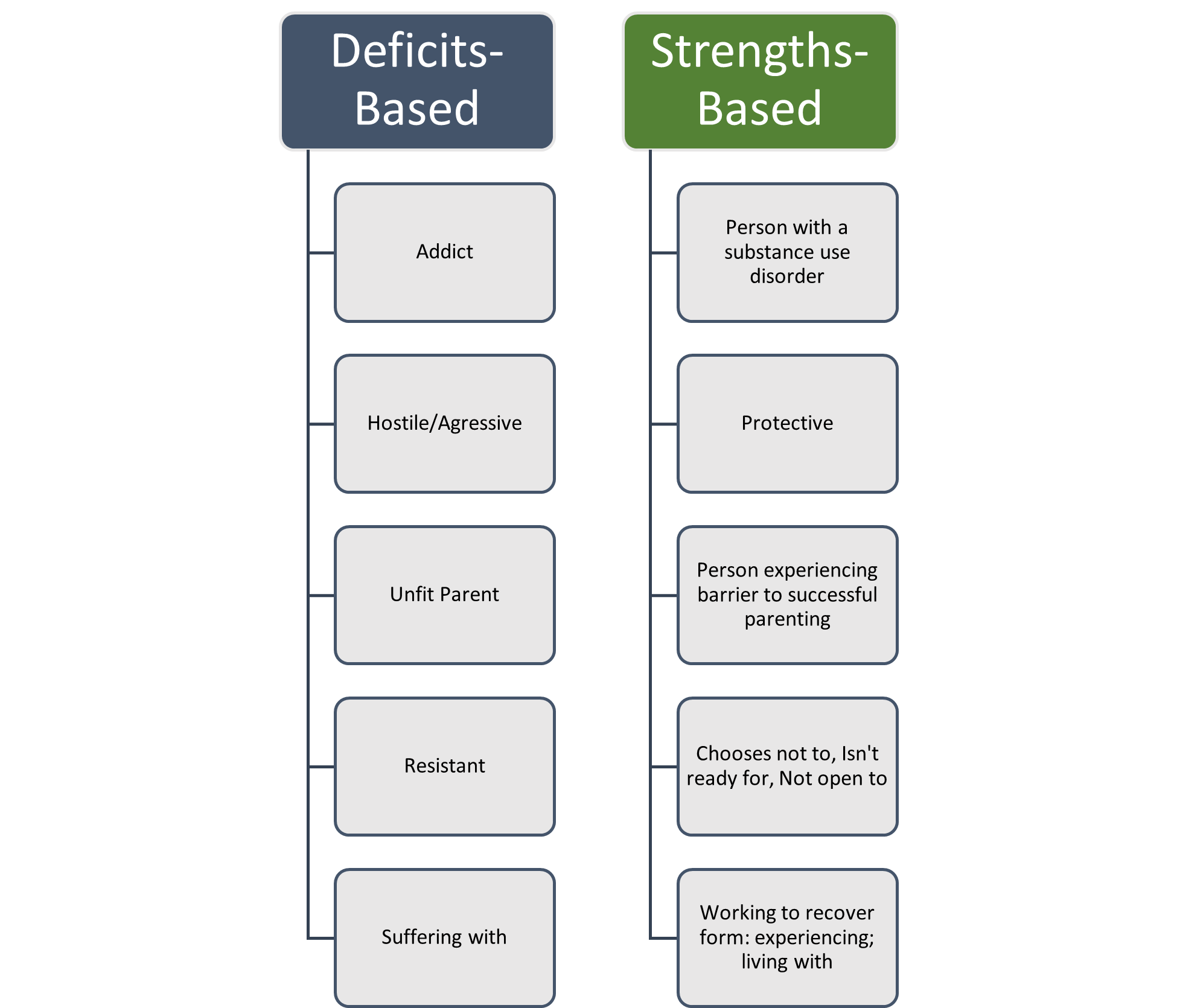
- Nursing Diagnosis or Problem/Strengths Statement (Please see Figure 3 for examples of strength-based statements)
- Planned interventions
- Client outcomes (i.e., response to interventions)
- Evaluation
Figure 3. Examples of Strength Based Documentation (https://positiveexperience.org/)
Data Collection: THEO
THEO, short for Tracking Home Visiting Effectiveness in Oregon, is a comprehensive data system designed to gather and manage home visiting data for the Babies First! and CaCoon programs. The guidance manual for THEO can be found here. This manual was created to help you learn how to use the THEO data system. For questions or to give feedback, please contact THEO Application Support (see below). This initiative serves to monitor the effectiveness and outcomes of home visiting interventions in the state of Oregon. The data collection process involves various surveys, totaling six distinct forms:
-
Enrollment
-
Every Visit
-
Infant/Child
-
Child/Youth (CaCoon only)
-
Caregiver
-
Disenrollment
These forms are available in English and Spanish on the THEO website.
While these forms are referred to as "surveys," they are not to be read aloud to clients; instead, data should be extracted from interactions and therapeutic communication during home visits. The surveys cover a range of topics related to client demographics, participation, health history, and other relevant information. The system also has features to track appointments, monitor visit outcomes, and compile deidentified reports for analysis. Data accuracy and timely entry are encouraged, with regular data entry expected within 10 business days of each visit.
For questions or to give feedback, please contact THEO Application Support.
Billing Documentation: Targeted Case Management
If you are submitting a TCM claim, TCM activities (assessment, plan, referral and monitoring) must be well documented in the medical record for the date of service on the claim. Use of the OHA TCM Assessment, TCM Service Plan, and TCM Visit forms is highly recommended. If using an electronic charting system, please ensure all data elements from the forms are captured and easily retrievable for auditing purposes. TCM Documentation Guidance is included in the TCM FAQ (starting page 4). For more information on TCM, see
Chapter 4.
Return to Top
Required administrative policies:
LPHAs are required to have administrative policies addressing the following subjects:
- Referrals and intake process
- Home visitor safety/Emergency Preparedness:
- Policy must ensure training is provided to all program staff.
- Consent for services and data collection:
- Policy, procedures and practices must ensure that the informed consent process is provided verbally and accompanied by written materials for each client enrolled in the program. It must be presented in a language and style that the client understands. Enrollment in nurse home visiting programs is voluntary, and that wording must be included in the consent. Families may choose to discontinue services at any time.
- Policy, procedures and practices must ensure that consent is obtained from every client allowing for data about their home visiting experiences to be maintained in the electronic data collection system (THEO). The consent form must include assurance that all data about the family used for reporting and/or evaluation purposes will be de-identified and aggregated, and that no identifying data will ever be made public. The consent form informs the client that records review is limited to specific agency staff providing the Home Visiting services to the family. Clients must be provided with information regarding local privacy practices to meet requirements of the Health Information Portability and Accountability Act (HIPAA).
- Data collection and reporting:
- Policy, procedures and practices must ensure that Home Visitors collect required data on client visits and enter it into the state-designated data system in a timely manner that is aligned with expectations defined by each program and within no more than thirty (30) business days of visiting the client and 45 days of case closure.
(PE-42)
- Social media use and texting
- Chart review policy:
- Policy, procedures and practices must ensure that four charts are reviewed per home visitor per year (peer chart review by a nurse is acceptable for the purposes of quality assurance).
- Mandatory reporting:
- Policy must ensure training is provided to all program staff.
- Medical records and confidentiality:
- Policies, procedures and practices must ensure confidentiality of client information in accordance with policies of the Health Information Portability and Accountability Act (HIPAA), including electronic protected health information (ePHI).
- Cultural safety and linguistic responsiveness
- Service for persons with disabilities
- Communication with persons with limited English proficiency
State Program Reviews:
OHA – Triennial Review
The triennial review is conducted every three years during which each of Oregon's 34 Local Public Health Authorities (LPHAs) is reviewed by the Oregon Health Authority, Public Health Division (OHA, PHD) to assess compliance or quality assurance, or both, with state, federal and other contract requirements for providing public health services. Review schedules and guidelines are managed by the OHA Director's office in collaboration with the LPHA Administrator. The Maternal and Child Health Nurse Home Visiting program compliance is based on the
PE-42 contract. Program elements are reviewed for compliance using the MCH Babies First! Program Tool and the Babies First! Chart Review Tool, located on the
Oregon Triennial Review Website.
OCCYSHN – End of Year Report
OCCYSHN has combined the CaCoon Accountability Report and the Shared Care Planning End of Year Report for ease of reporting. The purpose of the report is to confirm your agency's accountability to the
CaCoon Standards and/or Shared Care Planning Contract and to provide the Oregon Center for Children and Youth with Special Health Needs (OCCYSHN) with information about the barriers that your staff encounters and factors that help your staff provide services to our population. The information that you provide in this report is confidential; only OCCYSHN staff will see the information. OCCYSHN may aggregate county Accountability Report and Shared Care Planning End of Year Report information to share with our Federal and state partners; however, neither you nor your county will be identified. OCCYSHN will use this information to confirm our accountability to our Federal partners and inform our work on behalf of children and youth with special health needs and their families. The report is sent to local leads in early fall every year via a RedCap link. It is typically due in early November.
Return to Top
Nurse Home Visiting Programs are most effective when they are integrated into the community. Babies First! and CaCoon are voluntary services, should be offered at no cost to the family, and families enter the program through referral. Sometimes these are self-referrals, but often they are from health and social service providers in the community. It is essential that community partners who also serve pregnant and parenting people and their children are aware of the program and know how to refer eligible clients into it.
This takes communication with community partners and efficient referral processes. Babies First! and CaCoon are part of a larger home visiting system; coordinated referral systems are encouraged.
Communication back to the referral source about contact with the newly referred client makes coordination of services easier. To do this, the client will need to agree to allow the information exchange. Smooth and coordinated referrals take thought and planning.
Local programs are required to have written policies about their referral policies and procedures that describe how the program will establish and maintain local community referral sources.Local referral policies should include at least the following referral guidelines:
- Clients are preferably contacted within 3 business days (up to 10) of receiving the referral.
- Clients will be contacted at least 3 times over the next four weeks to offer enrollment in home visiting services.
- If unable to contact after four weeks, a letter may be sent. If there is no response within two weeks of the letter being sent, the referral may be closed.
To encourage participation in the programs, consider the following
recommendations from Pew Charitable Trust (PEW) (10) when reaching out to families in your community:
- Research demonstrates that “home visiting" may be off-putting to some clients. Consider other suggestions that have been shown to appeal to clients, such as “family support and coaching" or “family support and advocacy."
- When speaking to prospective participants, highlight help with setting career and educational goals, reducing stress, and accessing services such as affordable day care.
- Produce literature for clients that is simple, personal, and to the point and stresses flexibility, with equal emphasis on the caregiver's and child's development.
For ideas for increasing referrals and enrollments, see
Appendix A: Client Enrollment.
Return to Top
9. Caseload Requirements and Recommendations
Both Babies First! and CaCoon programs rely on the expertise of Public Health Nurses (PHNs) to assess the strengths and needs of clients, develop collaborative care plans, oversee cases, and track progress towards set goals. To introduce a Babies First! or CaCoon Program within a community, it is recommended that the implementing agency maintains a staffing level of at least
one 0.5 Full-Time Equivalent (FTE) supervisor and
one 0.5 FTE PHN, catering to a minimum of 20 clients per year. While a preference is given to nurses holding a Bachelor of Science in Nursing (BSN) degree, it is not obligatory. If the local program falls short of staffing or caseload standards, it is advisable to engage with a Babies First! or CaCoon MCH Nurse Consultant for further dialogue.
The role of nurse home visitors in both programs encompasses more than just home visits. PHNs are required to prepare for visits, manage cases between visits, document interactions, engage in continuous education, participate in community meetings, partake in reflective supervision, attend case conferences and team meetings, and have access to sick and vacation leave. Given the diverse tasks of a PHN, their multifaceted responsibilities should be taken into account when determining productivity benchmarks. It is suggested that 60% of an FTE should be allocated to home visits (including travel and documentation), while the remaining 40% should cover other tasks like meetings (team meetings, case conferences), ongoing education, breaks, vacations, and sick leave. On average, a home visit, including travel and documentation, takes approximately 2 hours.
Programs may need to use county-specific travel times and telehealth usage to create county-specific expectations of productivity standards. A 1.5 hr/telehealth visit productivity guideline may be used. The 2 hrs/home visit guideline translates into the following productivity standards:
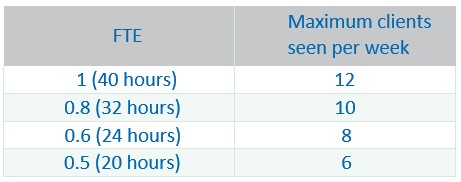
Note: 40 hrs/week * 60% of time for home visits = 24 hrs for visits/ 2 hrs per visit = 12 visits per week.
Best Practice:
The productivity standards are designed to strike a balance between community demands and a manageable nurse caseload that is safe for client and home visitor.
Determining an appropriate caseload for Babies First! and CaCoon home visitors is paramount to strike a balance between effective family support and preventing burnout. Caseload allocation considers the unique nature of these programs and their service delivery methods. These guidelines ensure the well-being of home visitors while providing optimal care to families.
Factors Guiding Caseloads
-
Family Acuity Level: Caseloads are influenced by the complexity of families served, ensuring a mix of varying acuity levels to prevent overwhelm and maintain care quality.
-
Full-Time Equivalent (FTE) Status: Caseloads correspond to the FTE status of home visitors. Part-time home visitors have proportionally adjusted caseloads to reflect their work hours.
-
Program Specifics: Caseload sizes align with the requirements and resources of Babies First! and CaCoon programs, adapting to their distinct goals.
-
Collaborative Resources: Collaborative distribution of caseloads across different roles, such as nurse home visitors and community health worker home visitors, ensures balanced workloads and optimal family support.
-
Service Delivery Mode: Caseload distribution considers whether visits are conducted in person at families' homes, at an office, or virtually. Remote home visitors may manage larger caseloads, while travel time impacts caseload requirements.
Guidelines in Practice
-
Balanced Caseloads: Maintain a balanced mix of families with varying acuity levels to prevent burnout and ensure effective support.
-
FTE and Program Dynamics: Caseloads align with home visitors' FTE status and specific program requirements, reflecting varying caseload sizes based on program needs.
-
Collaborative Synergy: Collaborate across roles to distribute caseloads effectively, maximizing resource utilization and enhancing family support.
-
Time for Administrative Duties: Allocate time for administrative tasks, including charting and documentation, to support accurate record-keeping and communication with other professionals.
-
Professional Growth: Offer ongoing professional development opportunities, such as trainings, conferences, workshops, supervision, and peer support. This investment fosters better outcomes for families and safeguards home visitor well-being.
Impactful Implementation
By adhering to these guidelines tailored to Babies First! and CaCoon home visitors, organizations create an environment that empowers home visitors to deliver optimal care. This approach ensures quality family support, while also preventing burnout by considering the well-being of home visitors.
A gradual ramp-up schedule for new nurse home visitors to attain optimal productivity is detailed in
Appendix C for both Babies First! and CaCoon programs.
Return to Top
10. Continuing Education
Babies First! and CaCoon home visiting staff are required to have an annual equity training according to the following guidelines:
- Two hours per year of continuing Equity Learning for all program staff is required
- Start with the mandatory Equity items listed in the Orientation Checklist
- For staff who have completed the orientation checklist Equity Learnings, two hours of continued Equity learning will be required every year from approved resources (see items 2 - 4).
- Learning may be in the form of self-paced articles or webinars or interactive trainings
- Approved learnings are listed in the MCH Resource Center under the Topic Area “Justice, Equity, Diversity, Inclusion and Belonging”
- Supervisors may request learnings be added to the Resource Center as approved Equity Learnings by filling out the feedback form.
- The list of approved learnings is fluid and dynamic; as we all learn and grow in equity work, approved learnings will change (see below for details)
- A vetting process for adding resources to the MCH Resource Center has been approved and will be used for all requests.
- Learnings are centered on (but not limited to):
- Anti-racism
- Trauma-Informed
- Intersectionality
- Anti-ableism training
- Disability Rights
- Disability Justice
- Reproductive Justice
- Supervisors will keep track of learnings of all staff and present a summary for Triennial Reviews.
Feedback Form
Please let us know if you have suggestions, any links are broken, or if any information is outdated.