The
988 Suicide & Crisis Lifeline is available 24/7. The Lifeline is for people in any type of behavioral health crisis, such as:
- Mental health-related distress,
- Thoughts of suicide or self-harm, or
- Substance use crisis.
People can get help by:
The Lifeline answers calls, texts and chats in English or Spanish, with interpretation services for more than 250 languages. People who are Deaf, Hard of Hearing or prefer using American Sign Language can
connect directly with a trained 988 counselor in ASL.
The Lifeline can also help people who worry that their loved may be in crisis.
The
988 Suicide & Crisis Lifeline connects people to trained crisis counselors who:
- Offer compassion, care and support.
- Connect people with the right kind of help, from the right type of helper.
To learn more, read these frequently asked questions about 988.
Other facts to know:
- People can connect with 988 through any phone or internet device in the United States.
- 988 routes callers by area code, not geolocation.
- Locked phones or phones that are out of prepaid minutes cannot connect to 988.
- Callers can press 1 to connect with the Veterans Crisis Line.
- Callers can press 2 for support in Spanish or text AYUDA to 988.
- Callers can press 3 for support for LGBTQIA2S+ youth and young adults or text PRIDE to 988.
Learn more about what happens when you use 988 through this infographic.

How Does 988 Work?
988 is different from 911. 911 focuses on sending in-person help to 911 callers. Meanwhile, 988 focuses on supporting the emotional health of callers.
- The Lifeline provides behavioral health care through compassionate, one-on-one conversations.
- Callers get emotional support in the moment they most need it.
988 counselors can ask for in-person help if the caller needs or asks for it. But often the call, text or chat is all people need to get through their crisis.
In Oregon, 988 resolves or de-escalates nearly 97 percent of calls over the phone.
- When an in-person response is needed, 988 call centers partner with Oregon's
Community Mental Health Programs, which can provide mobile crisis intervention teams with qualified behavioral health professionals.
- When a loved one or concerned citizen reaches out for help for someone in crisis, the first thing Oregon's 988 call centers do is try to talk to the person directly and offer emotional support. If that's not possible, 988 crisis counselors find out if there are any immediate safety concerns.
988 counselors do request support from emergency services when:
- There is clear risk of harm to the caller or others, and
- It is the only way to ensure the caller’s safety.
In most calls that need emergency services, the person in crisis has asked for this support. To learn more, read the 988 Suicide & Crisis Lifeline Suicide Safety Policy.
Vision for 988 and the Crisis Response System
988 is an exciting opportunity to reimagine how we respond to crisis
— in Oregon and the United States. The Oregon Health Authority (OHA) is working so that Oregon's crisis response system can:
- Offer people behavioral health responses to behavioral health crises.
- Respond in a way that is culturally, linguistically and developmentally appropriate.
- Provide trauma-informed care during crisis.
- Help people stay in their community.
- Meet the unique needs of groups disproportionately impacted by health inequities.
Longer term, OHA's vision is a robust system where:
- 988 is the first place people go for behavioral health crisis services.
- 988 links callers to local providers for a full range of crisis care services.
- 988 links callers to tools and resources that will prevent future crisis situations.
- People in crisis get the community-based care they need. They don't wait for care in emergency departments or jail.
This more robust system will be essential to meeting crisis care needs in Oregon.
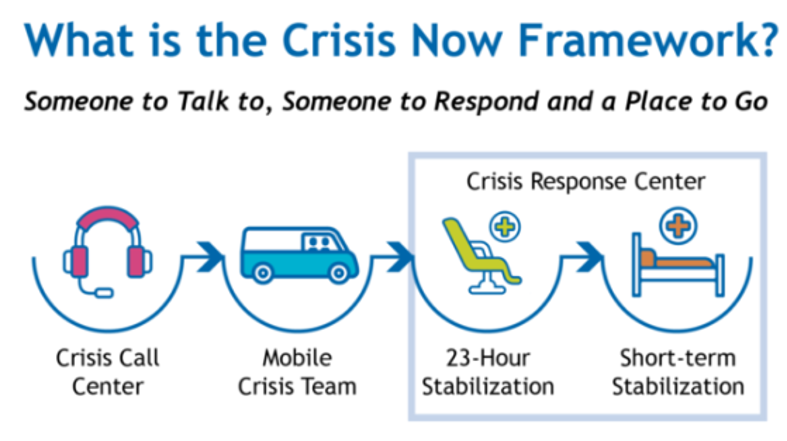
The "Crisis Now" Model for Adults:
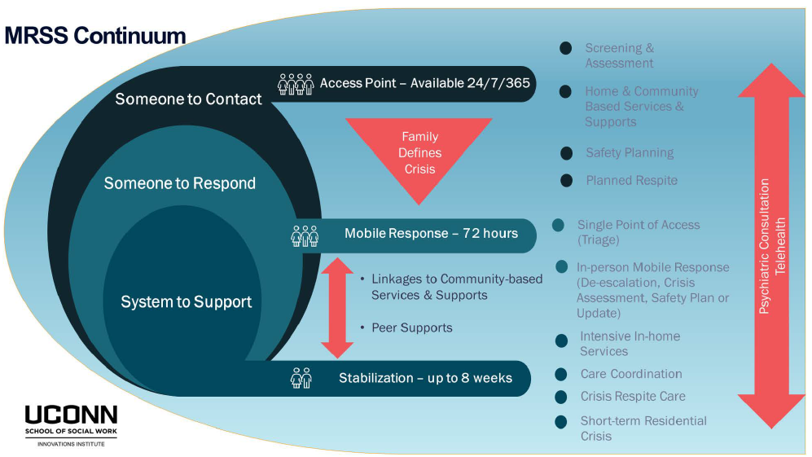
Mobile Response and Stabilization Services for Youth and Their Families:
To learn more, visit the Mobile Response and Stabilization Services page.
The most recent data from the Centers for Disease Control and Prevention show:
- In 2021, Oregon had the 17th highest rate of suicide in the United States with a total of 889 deaths. The Oregon rate of suicide has stayed well above the national rate since 2000.
- In Oregon, suicide is the second leading cause of death among youth aged 5-24.
Systemic and historical social injustice has harmed Oregon's crisis response system. In turn, this has harmed many with lived experiences and from disproportionately affected communities. They include groups such as:
- Youth
- Rural populations
- Communities of color
- Veterans
- People who serve or have served in the military
- Tribal communities
- People with disabilities
- People who identify as LGBTQIA2S+.
OHA understands that some people may not want to call an emergency or crisis number. This is especially true if they:
- Had an emotional or mental health crisis in the past.
- Were adversely impacted by systemic and historical social injustice.
- Were harmed or mistreated by police or health care systems.
This is why people with lived experience guide the future of Oregon's crisis response system.
- The Crisis System Advisory Workgroup (CSAW) provides an open community forum for people with lived experience to share feedback, questions and concerns about 988 and the Behavioral Health Crisis System in Oregon.
- House Bill 2757 (2023) requires a Behavioral Health Crisis System Advisory Committee, which includes consumers of adult behavioral health services, consumers of youth and family behavioral health services and other partners coming together to ensure coordination on improving the crisis system for all Oregonians.
- OHA convened a workgroup with the Association of Community Mental Health Programs (CMHP) to implement enhanced mobile crisis response services in each Oregon county.
- OHA offers a bi-monthly Learning Collaborative to provide a meeting space for peer-to-peer learning for CMHP providers developing Mobile Response and Stabilization Services (MRSS) and enhanced Mobile Crisis Intervention Services.
These groups work together to ensure quality mobile crisis response services throughout Oregon.
HB 2757 (2023) was passed to create a sustainable funding source for 988 call centers by implementing a $0.40 telecommunications fee, which will be used to help fund the call centers, including technology needs. These funds are required to be used for 988 call centers first, and any remaining funds can be used for mobile crisis services. This is expected to offset General Fund expenditures by $26 million in the 2023-25 biennium.
Approximately $118 million is currently invested for Mobile Crisis Intervention Services for the 2023-25 biennium for Community Mental Health Programs to enhance and expand mobile crisis services through enhanced Medicaid rates and County Financial Assistance Agreements.
Oregon Administrative Rule (OAR) Chapter 309, Division 72 outlines rules for mobile crisis intervention teams. These include:
- Requiring all counties to have two-person mobile crisis intervention teams available 24 hours a day, 7 days a week, to provide an in-person response. These teams include qualified behavioral health professionals. They may include peer support specialists and other health care providers such as nurses or social workers.
- Requiring all counties to offer Mobile Response and Stabilization Services for children, youth and young adults. OHA is requiring all counties to provide these services to eligible youth and their families, regardless of insurance status. OHA will continue to provide MRSS technical assistance and trainings to CMHPs and other providers in 2023 and beyond.